Sudden Cardiac Death/Ventricular Arrhythmia Risk In Atrial Fibrillation
Sudden cardiac death/ventricular arrhythmia risk was proportional to the number of independent risk factors.
The risk of sudden cardiac death (SCD)/ventricular arrhythmias is considerably higher in patients with atrial fibrillation (AF) compared with patients without AF, according to data recently published in Nature's Scientific Reports.
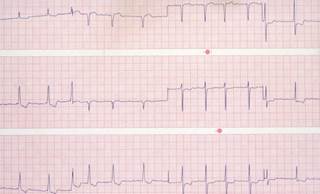
Researchers from Taiwan identified 352,656 patients with AF and 352,656 patients without AF from the National Health Insurance Research Database. The primary end points were defined as hospitalization or emergency department visit with SCD/ventricular arrhythmias (including ventricular tachycardia and ventricular fibrillation and flutter).
Baseline characteristics in the 2 patients groups were similar, with the exception of more comorbidities present in patients with AF. More than 23,000 patients experienced SCD/ventricular arrhythmias during a follow-up of 3,437,771 person-years (patients with AF, n=14,221; patients without AF n=9360).
There was a higher annual risk for SCD/ventricular arrhythmias in patients with AF (0.97%) vs patients without AF (0.47%). Patients with AF also had a higher risk for SCD/ventricular arrhythmias during the follow-up period (adjusted hazard ratio [HR] 1.64; 95% CI, 1.60-1.69). After considering age, sex, and comorbidities in a competing-risk model, patients with AF still had an increased risk for SCD/ventricular arrhythmias (adjusted HR 1.72; 95% CI, 1.67-1.77; P <.001).
Furthermore, AF was consistently associated with an increased risk for SCD/ventricular arrhythmias in different subgroups of patients, particularly younger patients (<75 years; P interaction <.001), patients who had end-stage renal disease (P interaction .001), malignancy (P interaction =.009), autoimmune disease (P interaction =.011), liver cirrhosis (P interaction =.025), and patients without hypertension (P interaction <.001); previous stroke/transient ischemic attack (P interaction <.001); or vascular diseases (P interaction <.001). SCD/ventricular arrhythmia risk was also higher in patients with AF who were not taking class I/III antiarrhythmic drugs and digoxin (n=252,843) compared with patients without AF (adjusted HR 1.66; 95% CI, 1.60-1.72).
Congestive heart failure, hypertension, diabetes, previous stroke/transient ischemic attack, vascular diseases, chronic kidney disease, and chronic obstructive pulmonary disease were determined to be independent risk factors for SCD/ventricular arrhythmias in patients with AF who were ≥75 years of age. The researchers found that the risk of SCD/ventricular arrhythmias was proportional to the number of risk factors a patient had. For example, having 1 risk factor would amount to an HR of 1.68 (95% CI, 1.54-1.84) increasing to 8.75 (95% CI, 6.92-11.08) for having all 8 risk factors compared with patients who had no risk factors.
“[C]linicians should pay attention to the potential risk of SCD/VAs [ventricular arrhythmias] for AF patients with multiple risk factors, especially when patients experience episodes of near fainting or syncope,” the researchers wrote. “Whether more aggressive treatment and better control of blood pressure, hyperglycemia, and congestive heart failure could decrease the risk of SCD/VAs deserves further study.”
Study Limitations
- It is unknown whether AF was directly responsible for the higher risk for SCD/ventricular arrhythmias since patients with AF had more comorbidities than patients without AF
- No data were available on AF subtypes; therefore, investigators were not able to determine whether the risk of SCD/ventricular arrhythmias was different for paroxysmal vs nonparoxysmal AF
- Since the diagnosis of SCD/ventricular arrhythmias was made on the basis of diagnostic codes in the database, the real incidence may be underestimated
- Age is a continuous variable
- All patients were Taiwanese; therefore, whether these results can be generalized to other populations remains to be seen
Story Credit: http://www.thecardiologyadvisor.com/atrial-fibrillation/afib-increases-risk-of-scd-and-ventricular-arrhythmias/article/655445/


