Hypertrophic Cardiomyopathy
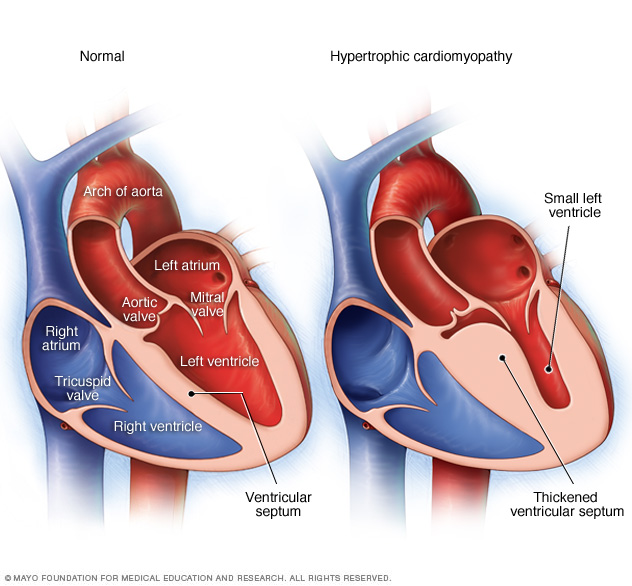
Illustrations of a normal heart (left) and a heart with hypertrophic cardiomyopathy (HCM). Note that the heart walls (muscle) are much thicker (hypertrophied) in the HCM heart.
Overview
Hypertrophic cardiomyopathy (HCM) is a disease in which the heart muscle (myocardium) becomes abnormally thick (hypertrophied). The thickened heart muscle can make it harder for the heart to pump blood.
Hypertrophic cardiomyopathy often goes undiagnosed because many people with the disease have few, if any, symptoms and can lead normal lives with no significant problems. However, in a small number of people with HCM, the thickened heart muscle can cause shortness of breath, chest pain or problems in the heart's electrical system, resulting in life-threatening abnormal heart rhythms (arrhythmias).
Symptoms and causes
Symptoms
Signs and symptoms of hypertrophic cardiomyopathy may include one or more of the following:
- Shortness of breath, especially during exercise
- Chest pain, especially during exercise
- Fainting, especially during or just after exercise or exertion
- Sensation of rapid, fluttering or pounding heartbeats (palpitations)
- Heart murmur, which a doctor might detect while listening to your heart
When to see a doctor
A number of conditions can cause shortness of breath and heart palpitations. It's important to get a prompt, accurate diagnosis and appropriate care. See your doctor if you experience any symptoms associated with hypertrophic cardiomyopathy.
Call 911 or your local emergency number if you experience any of the following symptoms for more than a few minutes:
- Rapid or irregular heartbeat
- Difficulty breathing
- Chest pain
Causes
Hypertrophic cardiomyopathy is usually caused by abnormal genes (gene mutations) that cause the heart muscle to grow abnormally thick. People with hypertrophic cardiomyopathy also have an abnormal arrangement of heart muscle cells, a condition known as myofiber disarray. This disarray can contribute to arrhythmia in some people.
The severity of hypertrophic cardiomyopathy varies widely. Most people with hypertrophic cardiomyopathy have a form of the disease in which the wall (septum) between the two bottom chambers of the heart (ventricles) becomes enlarged and impedes blood flow out of the heart. This condition is sometimes called obstructive hypertrophic cardiomyopathy.
Sometimes hypertrophic cardiomyopathy occurs without significant blocking of blood flow. However, the heart's main pumping chamber (left ventricle) may become stiff, reducing the amount of blood the ventricle can hold and the amount pumped out to the body with each heartbeat. This condition is sometimes called nonobstructive hypertrophic cardiomyopathy.
Risk factors
Hypertrophic cardiomyopathy is usually inherited. There's a 50 percent chance that the children of a parent with hypertrophic cardiomyopathy will inherit the genetic mutation for the disease. Close relatives — parents, children or siblings — of a person with hypertrophic cardiomyopathy should ask their doctors about screening for the disease.
Complications
Many people with hypertrophic cardiomyopathy (HCM) don't experience significant health problems. But some people experience complications, including:
- Arrhythmias. Thickened heart muscle, as well as the abnormal structure of heart cells, can disrupt the normal functioning of the heart's electrical system, resulting in fast or irregular heartbeats. Atrial fibrillation, ventricular tachycardia and ventricular fibrillation are among the arrhythmias that may be caused by hypertrophic cardiomyopathy. Atrial fibrillation can also increase your risk of developing blood clots, which can travel to your brain and cause a stroke.
- Obstructed blood flow. In many people, the thickened heart muscle obstructs the blood flow leaving the heart. Obstructed blood flow can cause shortness of breath with exertion, chest pain, dizziness and fainting spells.
- Dilated cardiomyopathy. Over time, thickened heart muscle may become weak and ineffective in a very small percentage of people with HCM. The ventricle becomes enlarged (dilated), and its pumping ability becomes less forceful.
- Mitral valve problems. The thickened heart muscle can leave a smaller space for blood to flow, causing blood to rush through your heart valves more quickly and forcefully. This increased force can prevent the valve between your heart's left atrium and left ventricle (mitral valve) from closing properly. As a result, blood can leak backward into the left atrium (mitral valve regurgitation), possibly leading to worsening symptoms.
- Heart failure. The thickened heart muscle can eventually become too stiff to effectively fill with blood. As a result, your heart can't pump enough blood to meet your body's needs.
- Sudden cardiac death. Ventricular tachycardia and ventricular fibrillation can cause sudden cardiac death. People with hypertrophic cardiomyopathy have an increased risk of sudden cardiac death, although such deaths are rare. Sudden cardiac death is estimated to occur in about 1 percent of HCM patients each year. Hypertrophic cardiomyopathy can cause heart-related sudden death in people of all ages, but the condition most often causes sudden cardiac death in people under the age of 30.
Diagnosis
Your doctor may review your medical and family history, discuss your signs and symptoms, and conduct a physical examination. Your doctor may order several tests to diagnose hypertrophic cardiomyopathy (HCM).
Your doctor is likely to recommend an imaging test called an echocardiogram to diagnose hypertrophic cardiomyopathy. This test allows your doctor to see whether your heart muscle is abnormally thick, your blood flow is obstructed and your heart valves are moving normally.
Types of echocardiography include:
- Transthoracic echocardiogram. In this test, a device (transducer) is pressed firmly against your skin. The transducer aims an ultrasound beam through your chest to your heart, producing moving images of the working of the heart.
- Transesophageal echocardiogram. In a transesophageal echocardiogram, doctors guide a flexible tube containing a transducer down your throat and into the tube connecting your mouth and stomach (esophagus). From there, the transducer can obtain more-detailed images of your heart. This test may be recommended if it's difficult to get a clear picture of your heart with a standard echocardiogram or if the doctor wants to further examine your mitral valve. This test is done in very few people with hypertrophic cardiomyopathy.
Additional tests might be ordered to look for other effects of hypertrophic cardiomyopathy and help your doctor determine the most appropriate treatment for your condition. These additional tests include:
- Electrocardiogram (ECG). Wires (electrodes) attached to adhesive pads on your skin measure electrical impulses from your heart. An ECG can detect enlarged chambers of your heart and abnormal heart rhythms.
- Treadmill stress test. Your heart rhythm, blood pressure and breathing are monitored while you walk on a treadmill. Your doctor may recommend a treadmill stress test to evaluate symptoms, determine your exercise capacity, and determine if exercise provokes abnormal heart rhythms. Treadmill stress tests are sometimes performed with echocardiography if you have symptoms of HCM but a resting echocardiogram doesn't show obstructed blood flow. This test is commonly used in people with hypertrophic cardiomyopathy.
- Holter monitor. You may wear a portable ECG that records your heart's activity continuously over one to two days. This test is often done in people with hypertrophic cardiomyopathy.
- Cardiac MRI. A cardiac MRI uses magnetic fields and radio waves to create images of your heart. Cardiac MRI is often used in addition to echocardiography in the evaluation of people with hypertrophic cardiomyopathy.
- Cardiac catheterization. In this procedure, a catheter is inserted into a blood vessel, usually in your neck or groin area. The catheter is then carefully threaded to your heart chambers under guidance of an X-ray machine. In addition to measuring pressures in your heart, cardiac catheterization is used to obtain X-ray images (angiograms) of your heart and blood vessels. A dye is injected through the catheter to help visualize your heart and blood vessels. This test is rarely used to diagnose hypertrophic cardiomyopathy.
Family screening
If you have a first-degree relative — parent, sibling or child — with hypertrophic cardiomyopathy, doctors may recommend that you be screened for the condition. Doctors will discuss with you the test results, and the risks and benefits of genetics tests. There are two types of screening:
- Genetic testing. Genetic tests may not provide a definitive answer because the genetic causes of hypertrophic cardiomyopathy aren't fully understood. Only 50 to 60 percent of families with HCM have a currently detectable mutation, and some insurance companies may not cover genetic testing. However, if an abnormal gene is detected in your family, then other family members can learn if they are at risk of hypertrophic cardiomyopathy through genetic testing. Consultation with a genetic counselor is recommended to help you determine whether genetic testing is a good option for you.
- Echocardiography. If genetic testing is not done, or if the results are not helpful, then your doctor may recommend echocardiography on a regular basis if you have a family member with hypertrophic cardiomyopathy. Adolescents and competitive athletes should be screened once a year. Adults who don't compete in athletics should be screened every five years.
Treatment
The goal of treatment is to relieve symptoms and prevent sudden cardiac death in people at high risk. Specific treatment varies depending on the severity of your symptoms. Your doctor will discuss with you the most appropriate treatment for your condition.
The options include:
- Medication. You may be given medications to relax the heart muscle and to slow the heart rate so that the heart can pump more efficiently. Your doctor may recommend beta blockers such as metoprolol (Lopressor, Toprol), propranolol (Inderal, Innopran XL) or atenolol (Tenormin), calcium channel blockers such as verapamil (Verelan, Calan, Covera-HS) or diltiazem (Cardizem, Tiazac, Dilacor XR), or medications to control your heart rhythm such as amiodarone (Cordarone, Pacerone) or disopyramide (Norpace). If you have atrial fibrillation, your doctor may prescribe blood thinners such as warfarin (Coumadin, Jantoven), dabigatran (Pradaxa), rivaroxaban (Xarelto) or apixaban (Eliquis) to reduce your risk of blood clots.
- Septal myectomy. A septal myectomy is an open-heart procedure in which the surgeon removes part of the thickened, overgrown septum between the ventricles. Removing part of this overgrown muscle improves blood flow and reduces mitral regurgitation. Surgeons may conduct this procedure using different approaches, depending on the location of the thickened heart muscle. Surgeons may sometimes perform mitral valve repair at the same time as a myectomy. A myectomy may be recommended if medications don't relieve your symptoms. Most people who have a myectomy have no further symptoms. Septal myectomy is available only in medical centers that specialize in the treatment of hypertrophic cardiomyopathy.
- Septal ablation. In septal ablation, a small portion of the thickened heart muscle is destroyed by injecting alcohol through a long, thin tube (catheter) into the artery supplying blood to that area. This procedure may improve your symptoms. Possible complications with this procedure include heart block — a disruption of the heart's electrical system — which requires implantation of a pacemaker.
- Implantable cardioverter-defibrillator (ICD). Doctors may recommend an ICD if you have life-threatening heart rhythm disorders (arrhythmias) such as ventricular tachycardia or ventricular fibrillation. An ICD is a small device that continuously monitors your heartbeat. It's implanted in your chest like a pacemaker. If a life-threatening arrhythmia occurs, the ICD delivers precisely calibrated electrical shocks to restore a normal heart rhythm. Your doctor may recommend an ICD if you have hypertrophic cardiomyopathy and you're at high risk of sudden cardiac death because of abnormal heart rhythms.
Story Credit: http://www.mayoclinic.org/diseases-conditions/hypertrophic-cardiomyopathy/home/ovc-20122102


