Regina Welkie

Regina Welkie is a physician assistant in the Lehigh Valley region of Pennsylvania and has experience in surgery, internal medicine, and gastroenterology. Regina is also a faculty member in the DeSales University Physician Assistant Program in Center Valley, PA. She has a condition called Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC), a genetic heart condition associated with cardiac arrhythmias and sudden cardiac death and lives with an internal cardioverter defibrillator (ICD). Regina said the perspective she gained from being a patient with a cardiac condition truly changed her life and the way she practices medicine and educates her students.
Reginia realized she is fortunate to be alive and share her story. She hopes to use this amazing gift to be an advocate for others with heart conditions. Regina is excited to use her platform as a physician assistant and PA educator as well as a patient to bring awareness to arrhythmia syndromes and their significant roles in cardiac arrest and sudden cardiac death in young people. She hopes to convey the importance of recognizing symptoms and being persistent in reporting them.
"I am looking forward to being part of the SafeBeat Initiative to promote screening for cardiac conditions even before symptoms become evident and to save lives as a result!"
This is my story:
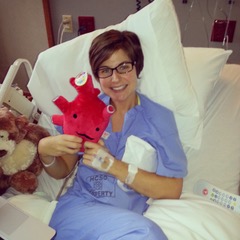
I was an athlete for most of my life. I played basketball, soccer, and ran track in school and as an adult had become an avid runner and cyclist. I initially began experiencing palpitations, difficulty catching my breath, and lightheadedness while exercising around the age of 32. I was evaluated by a physician and, as an otherwise healthy young woman, was felt at the time to have a benign arrhythmia likely related to anxiety and caffeine. I was reassured and, despite persistent and worsening symptoms, continued to exercise. My symptoms became more frequent and several times while running or cycling I would develop pounding in my chest and episodes of near fainting which required me to stop and even lie down. I voiced these complaints to my primary care physician who ordered a 24-hour Holter monitor. The results of this test showed multiple episodes of ventricular tachycardia (VT) with heart rates as high as 260 beats per minute. I was urgently admitted to the cardiac ICU, underwent extensive cardiac testing, and was found on an MRI to have a scar on my heart which led to the arrhythmia. I had a cardiac ablation to target the arrythmia which, unfortunately, was unsuccessful and subsequently led to placement of an internal cardioverter defibrillator (ICD). At the time, the diagnosis remained unclear, so I was given permission to begin exercising again. I was placed in a cardiac rehab program and was doing well getting back into my routine. I was running on a treadmill during the last week of rehab and suddenly my chest started pounding and I felt dizzy. I heard the staff telling me to stop the treadmill and before I could take action, my ICD fired. Despite changes in activity and medications, I continued to have episodes of VT and was shocked by my ICD on another occasion while traveling in Europe. Recurrent arrhythmia led to further testing and procedures, including an epicardial ablation, which targeted the scar on the outside of my heart. The testing and procedures I underwent led to an eventual diagnosis of ARVC.
ARVC is a genetic heart condition which causes normal heart tissue to turn to scar and can lead to ventricular tachycardia and is an important cause of sudden cardiac arrest and sudden cardiac death. This condition often presents in young athletes given the strain on the heart during exercise and can be fatal if not recognized. Arrhythmias can worsen and disease can progress into heart failure with continued endurance exercise, so those diagnosed with ARVC are advised to restrict activity. Since this condition often presents in athletes, these restrictions become difficult to accept for so many with this diagnosis. Running and cycling were outlets to relieve stress for me and had become important aspects of my daily life and identity and to have these things abruptly taken away was challenging to overcome. It took significant time, patience, and unending support from providers, family, and friends.
I have since found ways other than running and cycling to remain healthy. I can be found most days walking with my goldendoodle, Ilsa, practicing yoga, or golfing with my amazing husband! ARVC is a chronic heart condition, so while I haven’t allowed this diagnosis to define me, it has become an integral part of the person I have become. While my life may now literally have a different rhythm than before my diagnosis of ARVC, I have learned to more fully appreciate the life I’ve been given, to live more mindfully, and ultimately to take better care of myself and my heart!
In addition to my own story, I'd like to share the heart story of another brave fighter in my family. My niece, Charlotte, is currently 7 years old and was born with a congenital heart defect called Shone's complex. She had open heart surgery soon after birth to fix a coarctation of the aorta and is thriving!! She is a sassy, spunky, and active 7-year-old who is full of laughter and life! This is why it’s so important to screening kids who may not be as fortunate to have the resources Charlotte had and who live with undiagnosed heart conditions.




